Aim: Safety, Quality, Equity ; Scale : City Wide ; Location : Mumbai ; Stake Holders : Multiple ; Lead Organisation : Open ; Duration: 3 years ; Visibility: Public .

We have ours eyes on excellence. The 20/20 Vision is not a limit but the beginning of a ambitious journey. The 20/20 Vision does not promise world-class health system but will uncompromisingly work towards embedding world-class capability for improvement and innovation, across the whole Healthcare Ecosystem of Mumbai. We are ambitious but realistic.By focusing on ‘Capabilities’ , we visualize a ‘System’ that is capable of transforming itself.
Laying the Foundation for World -Class Health System
A broad-based platform to support a maximum vision: A Community of Solutions.
The central aims of a ‘healthy’ health system is a commitment to safety, quality and equity. 
Building capabilities requires not merely the supply of value but the public must also be empowered to evaluate the quality and safety of the care provided. Supply of value is about technical efficiency; demand for value is about allocative efficiency. Healthcare should be targeted to those who need it most. Quality currently follows the money. It is money that should follow quality. Helping the public make well informed decisions is by creating greater transparency . Accountability requires transparency.
Theories of Improvement that have influenced healthcare policy making has been in two large conceptual groups. The focus on how healthcare is organised and delivered on the one hand . The second focus is how that delivery is financed and the incentives that motivate performance and productivity.
The methods motivating improvement of healthcare require measures that ensure public accountability for variety of outcomes but also greater collaboration and sharing of knowledge and experience within communities of practices.
These efforts are themselves dependent on innovative ways of managing knowledge and bringing together the various stakeholders to work synergistically. The problems of healthcare are challenging and cannot be solved without extraordinary alignment that connect the dots to provide a systemic framework for problem solving.
Purchasing , social accountability and regulation are on the demand side of the value creation equation while the organisation and delivery of care, communities of practice and deployment of knowledge constitute the supply side of the Value in Healthcare.
Re-imagining Healthcare for All.
Mumbai is a multi-layered city that accommodates disparity in wealth as a given , but why does it tolerate such a disparity in health. This is a question that every ones conscience should bear. Healthcare for all presupposes Healthcare Excellence for All: Access to unsafe, insufficient , incomplete, inappropriate care is waste of resources. If quality is guaranteed the public will access it at the appropriate level. Access is not an isolated problem but a design or system problem.
Universal Healthcare must be preceded by Universal Access to Digital Health, Personal Health Data, Health Insurance and access to Quality and Scale-up of Excellence.
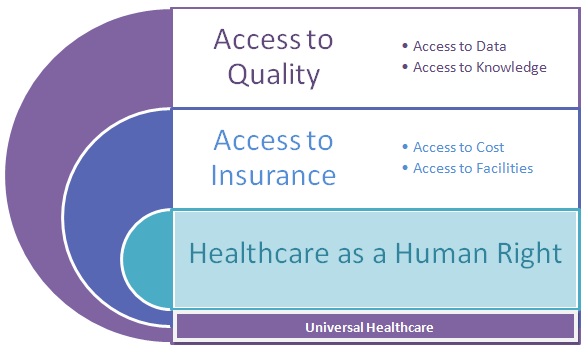
Will Mumbai become the first city to provide Equal Access to Quality Healthcare as a Human Right?
Twenty Worthy Aims for Mumbai Healthcare
maxiMUMcare is a campaign to maximise the contributions of healthcare to society.
- The main goal of any healthcare system is to get better and better at what it does. Continous improvement is no longer an ideal in healthcare , it is the basis of healthcare. The formal body of knowledge to improve performance is widely available. What remains to be done is creating the conditions that allow change to happen. This is not resource-intensive but participation-intensive.
- Accelerated Access: the first point of contact with the health system is highly variable , unpredictable and is constrained by ability to pay. Innovations in technology assisted consultations will pave the way for an fully engaged healthcare system. An ecology of care approach that allows flow to appropriate ‘ levels of care ‘ is an issue for design. Remote healthcare.
- Educate Clinical students for society . They should understand not just discipline domains but also about the system and the industry and society.
- Community Health Rights rather than merely patient rights.
- Recognise the limitation of regulation.
- Plan for sustainable consumption of healthcare . Linking universal healthcare intentions to resources without building capabilities for accountability and improvement would pave the way to crisis.
- No women in labour shall be turned away.
- Need for a seperate Healthcare Quality Fund publicly managed.
- Digital infrastructure : Maximise return on data.
What will Mumbai’s Healthcare look like in 2020 ?
The vision of 2020 is not an answer to the question of ‘Why?’ but to ‘Why-not?’: a judicious mix of Research and Future-Search. Campaign are not about ‘business- as- usual’ but about challenges that cannot be handled by individual organisations . So what will Mumbai’s healthcare quality system achieve.
A. Supply of Value
- A world class infrastructure of improvement that is made up of cohesive cluster of second- order institutions supported by a strong network of professionalized quality specialists that would be accountable to the public.
- Mumbai will become the Healthcare Quality Capital of India. We wish see a Certified Professional in Healthcare Quality in every hospital in Mumbai.
- A substantive Mumbai Healthcare Information Exchange that would promote democracy of data on individual , institutional performance and cost . Greater opportunities for Healthcare Data entrepreneurship.

- Equity of early access to reliable health guidance, regardless of ability to pay . Three Clicks away.
- Care Transition Management supported by cadre of case managers.
- Improvement Science integrated into the curriculum of clinical students .
- A innovation space for healthcare .
B. Demand for Value:
- A hyper -local community led plan for prioritization of healthcare resources.
- Health Rights monitored by the community. Community Health Rights
- A dash -board for evaluating the performance of the healthcare system with drill-down options.
- National Benchmark data-base that is geographically adjusted.
- Mumbai would become the first city to achieve universal access.
- Ongoing Needs assessment to help map the burden of disease.
- Public reporting of risk adjusted outcomes on voluntary basis and not merely increased utilization.
- A government supported ‘Agency for Patient Safety’ with mandatory incident reporting.
- Statutory protection for clinical evaluation activities such as Audits , Incident Reports, etc
- Insurance and TPA organisations to move towards Value Based purchasing.
- Greater Choice for Patients
C. Delivery of Care :
- Minimal or Early Care that is accessible, risk controlled and standardized with Evidence-Based Diagnosis and Referral Protocols to ensure ‘appropriate’ care ‘in time, every time’.
- Continuum of Care incentivized by strategic alliances between Hospitals and Community Care organisation.
- Socially vulnerable populations to receive a ‘Just Care’ at Secondary and Tertiary Levels.
- Uptake of Clinically -Relevant use of information technology.
- Use of Evidence Based Guidelines for larger number of Disease Conditions and Procedures.
- Clear distinction between care for Acute and Chronic conditions.
- Transparency of Outcomes and the use of competitive Benchmarks.
- Personal Electronic Health Records with secure access.
- Innovative Models of Care suited to the demographics and needs of the local population.
D. Financing of Healthcare:
- Insurance and TPA organisations would gradually migrate to Prospective- Payment Regimes.
- Disease- Specific insurance would be widely available for business- model innovation in Chronic Care .
- Clinical Code and Case-Mix based payments.
- Economic Disincentives for Never- Events.
- Incentives for Preventive Care practices.
E. Social Accountability:
- Accreditation would be the basic norm in both private and public healthcare system.
- Healthcare institutions would be more transparent and publically report their outcomes.
- An ‘Agency for Patient Safety’ would be in place to monitor harmful incidents.
- Comparable Cost of Care would be publically available .
- Track-able healthcare: Appointments , Test- Results, Waiting Time, Absenteeism .
F. Communities of Practice :
- Collaborative practices would be routine in Mumbai’s Healthcare.
- The public will have a greater share in participating in the design of healthcare programs.
- Healthcare would be treated as a inter-sectoral issue.
- A graduation based accreditation program MEDSTAR would facilitate further improvements in Clinical Quality.
G. Deployment of Knowledge
- Clinical student curriculum’s would include inter-professional electives in Improvement Science so that future training requirements in Healthcare Quality would be reduced.
- Best practices would regularly shared across the system.
- Post- Graduate courses in Healthcare Quality and Patient Safety would be available.
- Minimal and Primary Care would be based on Evidence- Based Guidelines.
F. Alignment of Forces :
- Continuity of Care for all.
- Greater role of social support interventions in improving outcomes.
- Levels of care approaches to guide redistribution of workload to appropriate levels.
- Effective Best Practices would be sustained and scaled up.
- Regionalisation of emergency and non emergency services.
- Healthcare Information Technology vendors would comply with inter-operability and data security standards.
The Bottom-Line:
maxiMUMcare is a Capability Campaign not an Outcomes Campaign. India has never had a SaveLives Campaign as it did not have the capabilities. By 2020 Mumbai’s Healthcare can hope to have one. The Campaign is determined to eliminate the ‘Capability Gap’ between Developed and Developing countries.
maxiMUMcare is a Capability Campaign not an Demonstration Project. Scale and Sustainability are inherent to maxiMUMcare.The campaign offers direct impact on daily- work and substantial incentives for individuals and organisations for participation.
maxiMUMcare is a Capability Campaign not a Resource- Dependent initiative. The maxiMUMcare campaign is innovation on the front-end of healthcare not on the back-end hardware of healthcare. Resources are finite. Capabilities are unlimited. Improving Quality while reducing Cost requires capabilities not more resources.
