Executive Summary
I. Introduction
II. Why do we need a ‘Capability for Improvement’ campaign?
III. Who can ‘improve’ the quality of Mumbai’s health system?
IV. What is required of participants?
A. Individual
B. Institutional
C. Public
V. What is the campaign methodology?
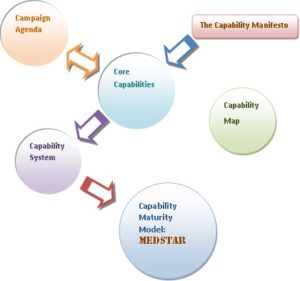
A. The Capability Manifesto
B. Campaign Agenda.
C. Why focus on ‘Capability’?
D. Campaign : Core Capability.
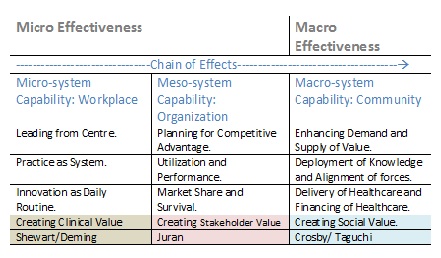
E. TripleAgenda Vs Triple Capability.
F. Matching Capability and Interventions
G. Capability System.
H. Improvement Capability Model.
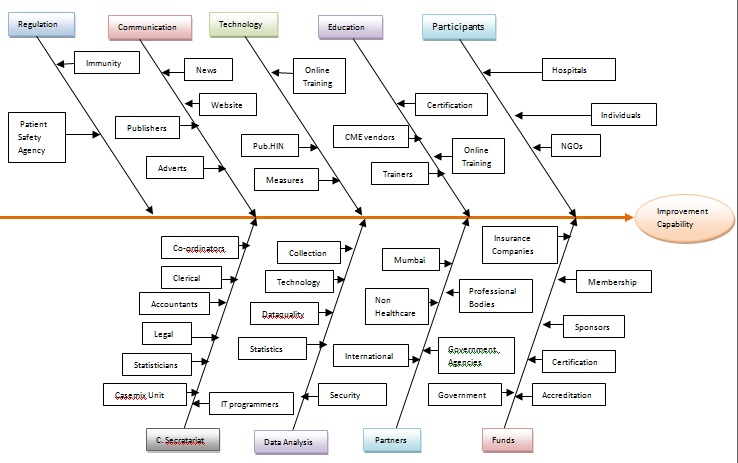
VI. Campaign Infra-structure and Timeline.
VII. Conclusion.
Appendix

Why do we need a Campaign to create ‘capabilities for improvement?
maxiMUMcare is a campaign to bring all the players- both private and public- on a common forum to transform Mumbai healthcare system, using scientific knowledge.
Access, Equity and high cost are problems common to all health systems in the world. It is customary to blame the government for these ills. Any attempts to improve the situation are seen as the responsibility of the authorities. While such ‘agency- based ‘interventions are still required, there is much that can be achieved by a ‘practice- based’ approach.
We all know the ‘problems of healthcare’ in Mumbai are and we have known them for so long. The maxiMUMcare campaign aims to focus on the ‘solutions for healthcare’ by recognizing current efforts as an asset and to leverage these efforts using modern theories and methods of healthcare improvement and technologies of transformation.
maxiMUMcare is unique in being a time-bound social experiment, that is voluntary and open to all. We believe it requires only 18 months of rigorous, multifaceted, collaborative effort to change Mumbai’s healthcare.
There is nothing that is ‘wrong’ in Mumbai’s healthcare that what is ‘right’ in Mumbai’s healthcare cannot solve. The campaign borrows assets that are already doing well and hopes to create a ‘community of solutions’.
Who can improve healthcare?
No one person, profession or institution can improve healthcare, whether it be a workplace, healthcare organization or an entire region. Everyone must work together to change the whole system. The knowledge and methods of improvement have to be learnt and are learnt best by doing. The campaign hopes to offer the necessary ‘knowledge base’ to its participants, through a network of world-class partners. Professional Development through CME credits and Certification possibilities are also under consideration. Read More.
The core mechanism of the campaign is a scientifically designed Fast- Break Series of collaborative that will aim at targets established by a broad-based ‘Healthcare Prioritization Council’.
Typical topics likely to be included in the Fast-Break Series, could be:
Peri-natal Capability Collaborative.
VTE Capability Collaborative.
Hand Hygiene Capability Collaborative.
End- of- Life Capability Collaborative.
Blood Conservation Capability Collaborative
See Appendix 2 for more extensive list of potentials collaborative topics.
A detailed blueprint of the Peri-natal Capability Collaborative is included as ‘Proof of Concept.’ [Appendix 2]
While ‘vital statistics ‘are good and necessary, they are insufficient to support improvement campaign. The underlying driver of the campaign is the availability of accurate, meaningful and actionable data. We are seeking technology and analytics partners who would establish a common, reliable and secure informatics structure that would provide quality data for the participants.
No campaign can be complete without public participation. Healthcare is always political. The campaign requires the ongoing support of socially committed media groups and advertising agencies.
Many of the issues central to the campaign are already being address by government and non governmental agencies. The campaign hopes to add value to their efforts by bringing them together and intensify their efforts together
Hospitals, nursing homes and other healthcare organizations that are members of the campaign would automatically become eligible for a unique graduation- based, accreditation program: MEDstar.
For other benefits to individual and organizational participants:
What is required of participants?
Individual Requirements:
Healthcare professionals are always short of time. Those participating in the campaign would thus receive just-in- time training, supported by self paced online courses.
We however foresee a demand for professionals dedicated to improvement science. These professionals would be invited to join the ‘Healthcare Quality Professional Network’ and would receive more advanced and career enhancing training.

As much of the training is likely to be subsidized, it is mandatory that participants agree to publication of the studies by iHQ.
As we anticipate intensive training over the 18 month duration, the campaign is likely to organize Test Prep programs for CPHQ and ABMQ. These programs are optional and may require a nominal additional fee. Exam fee are the responsibility of individuals.
Participant can enroll for minimum of one and maximum of three collaborative. Additional participation would be charged at a premium.
Note : Individual Membership in the campaign is not transferable and non refundable.
Institutional members
Quality and safety are not merely a public health issue but requires system improvements in organizations. All institutional members would automatically receive MED* [level 1 designation] once they qualify for participation.
What is the Campaign’s methodology?
The campaign is based on easily learnable, practical knowledge that is referred to as Improvement science. The campaign does not aim to achieve ‘world-class healthcare’ but ‘world-class capabilities for improvement ‘.
Improvement Capabilities are about new ways of doing things. They are driven by optimism. They begin with need but evolve into possibilities. Capabilities are not about managing the present, but about selectively forgetting the past and creating the future. The campaign is to demonstrate that there is an opportunity and the method for Mumbai health care to be better.
A judicious mix of education, collaborative based action, community engagement and reliable campaign infrastructure is our recipe for creating systemic momentum for change and improvement.
Campaign Agenda:
Equitable Access Quality and Safety Cost-Effectiveness
While it is possible to address all three elements of the agenda by one- off interventions , probably in isolation. The campaign motivates to learn and build shared capabilities that are sustainable without external support.
Why focus on ‘capability for Improvement’?
Improvement science is often seen as a collection of methods, models. systems and an underlying theory. As such project based improvement, including collaboratives, have been shown to produce results for those who can afford it. Capability is required if such efforts are to be sustained and scaled up. Thus we prioritize capability before method.
Capability refers to the conditions that make improvement possible. Unlike quality that is a competitive or rivalrous good, capability is a common or collaborative good. Everyone has an equal right to improvement capabilities. Methodologically capability treats problems as design issues.
The basic assumption underlying a capability approach is that the quality of care depends on the quality of the data, systems and improvement resources of healthcare organizations.
For further details : Read THE CAPABILITY MANIFESTO on page .
Campaign Agenda and Core Capabilities:
In a sense we do not think about capabilities while providing care. It is a second- order activity that is central to providing quality care. Capabilities are interrelated and work as a system. Capability approach views ‘ problems’ as design issues and provides safe- space for creativity. The convergence of the dimensions of quality and a focal point in creating a ‘ culture of healthcare improvement’.
iHQ’s Core Capability :
System Assurance Need/Outcome Analysis Value Creation
Capabilities are the basis of improvement science. It is not about context but the conditions of improvement. Improvement science is a field that is not afraid of numbers and actually embraces scale. Yet its methodologies are small and gregarious. It’s is not a ‘State’ science that flows from and follows authority, but a ‘nomadic’ science that de-territorializes problems, disciplines and organizations. It is these strengths that can turn into its weakness depending on the context. Capabilities are not about fixing the broken system they are about creating the future.
Developing countries face a paradox as they need the most to improve but have the least capabilities. Merely providing didactic ‘knowledge of Improvement’ is unlikely to lead to transformation of practices. It is this paradigm- gap that the campaign wishes to bridge. The focus on ‘capability’ shifts the focus of learning from ‘ learning about’ to ‘ learning to be ‘.
System Assurance: Needed structures: meeting the needs.
Definition of quality: How the whole system relates to an individual.
Systemness is a resource of care. The collective intention is prerequisite regardless of actual outcomes. In healthcare unlike in industry, the system is more than instrumental function , its is constitutive. At the least, it is the new placebo. If the aim of the system meets the need of the people. Reduce systemic alienation. When system , data and values are aligned.
When you ask what am I a part off rather than what can I do ? simplicity is system property where there is synthesis. What matters to you? Anticipation.
Problems don’t recur. Hope. The system is changeable. Freedom.choice. easiest way is co design. Patients and significant others contribute not only to process but to the quality of that process.
The view of the whole system is no longer the prerogative of the ‘top brass’ or the policy analysts but of frontline worker and the individual seeking the system for services.
System assurance views healthcare as a subsystem of society.
Systemness changes with domain.
New models of care and burden of disese
Knowing how you are doing ?
Pedagogy of Change : Systems Thinking
What is the ‘significance of systems’ in healthcare?
Need/ Outcome Analysis: Needed data and Decisions: who does what for whom at what cost.
Definition of quality: Match between voice of the process and voice of the customer.
Knowing what you are doing ? what works when?
Pedagogy of Change : Statistical Thinking
Simple Complex
Short term Community Tertiary
Long term Community Community
Value Creation: Needed action: reaching the unreached.
Definition of quality: The unconditional promise to continuously improve. The unconditionality is to improve without additional cost, if not with reduction of cost. It is the will to change.
Is cost an outcome.
Who needs what from whom? What is it we are paying for ? Closing gap between what we have and what
Pedagogy of Change : Improvement Thinking.
Use rapid results.
The Pedagogies of Change
The name of the game is change . Improvement requires managing both the demand and supply of systems , data and value. Currently there is a ‘capability deficit’ in all three fronts.
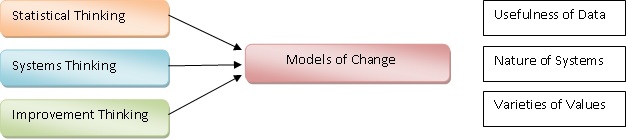 It maps the Juran’s trilogy as needs / outcomes is quality planning ; system assurance is quality control and value creation is quality improvement. The triple capabilities require three distinct though dependent pedagogies of change : Systems Thinking to guide systems assurance. Statistical thinking to guide actionable data on needs and outcomes and Improvement thinking to foster value creation.
It maps the Juran’s trilogy as needs / outcomes is quality planning ; system assurance is quality control and value creation is quality improvement. The triple capabilities require three distinct though dependent pedagogies of change : Systems Thinking to guide systems assurance. Statistical thinking to guide actionable data on needs and outcomes and Improvement thinking to foster value creation.
The Practice Science Model: Meta-Effectiveness PDCA
Improvement is a science of effects. Current models of models of improvement are not integral to care. The first generation of models were largely ‘work break down’ oriented and thus were explicit about the cross-functional nature of improvement activities. The second generation models were again largely developed outside healthcare and focused on micro-epistemologies involved in improvement activities. However both these models view the process of improvement as external to care.

Improvement is the new accountability. Instead of a standard- based system we now have an improvement- based system.
Meta- Effectiveness Model is about achieving ‘systemic effectiveness’ or ‘Systemness’. It is a model specific to healthcare. Accountability or system is usually seen as a process of standardization. In the meta-effectiveness model, there is no need for prior standardization . Standardization is a intermediary of improvement.
In this model , the first effect is based on doing the right thing . Its focus is on ‘cause- effect relationship’. It moves from efficacy to effectiveness or from controlled to uncontrolled context. It addresses the science- practice gap or knowing –doing gap. It is a mechanistic or structural intervention. It adopts a linear view of time. The goal post is fixed. Improvement is a applied science.
There are however two modes of execution of this phase based on whether there is an existing system or a new evidence- based system is being designed. In the former case the PDCA cycle begins with the check quadrant i.e. the test becomes a CAPD cycle in this case. In the case of new system design regular PDCA cycle is used.
The second effect is based on doing things right. It’s focus is on need- effect relationship. Learning can occur only by doing the right thing right. The degree of experimentation is enlarged. It is a process of creative research or improvisation. This a process of spiral or temporal reinvention. The goal post is constantly shifting. It is practice science.
The third effect is the best practice effect. It is ‘transfer of learning’ process. It a process of serial or spatial reinvention. The goal post is fixed. This PDSA starts with act. Thus it is an APDS cycle.
The last two focus on the doing- knowing gap. The ‘do’ of the first cycle , the ‘act or adapt’ of the second cycle and the study of the third cycle provide the ‘ varieties of effects’.
The final link is the practice- driven research. It is sometimes referred to in the literature as change- based research.
Currently all four phases are not as prevalent as they should be and remain eclectic at best.
The triple effect PDCA model allows for three modes of evidence utilization in an integrated manner. The first mode is the generalization mode that large depends on the external validility of the data. The second mode is one of localization . The third mode is one of provincialisation. Both localization and Provincialisation depend on the ‘quality of inference’. Localisation depends on the quality of data.
Matching effects, capabilities and Pedagogies 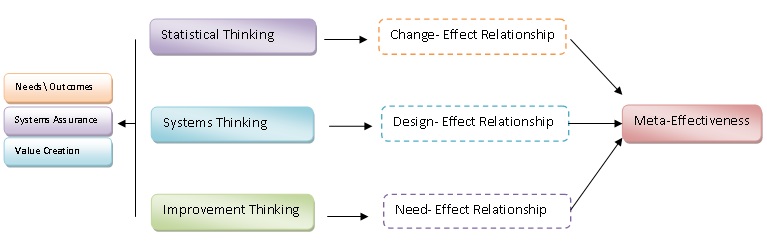 Meta-effectiveness is a system of effects. From a core focus on systems, data and need meta-effectiveness is a multi-dimensional understanding of effectiveness. While there is no effect without cause, the focus is not on determining merely linear cause – effect relationships as in traditional research , but in enhancing the inter-relationships between effects. Capabilities increase the demand and supply of data, the demand and supply of systems and the demand and supply of value.
Meta-effectiveness is a system of effects. From a core focus on systems, data and need meta-effectiveness is a multi-dimensional understanding of effectiveness. While there is no effect without cause, the focus is not on determining merely linear cause – effect relationships as in traditional research , but in enhancing the inter-relationships between effects. Capabilities increase the demand and supply of data, the demand and supply of systems and the demand and supply of value. 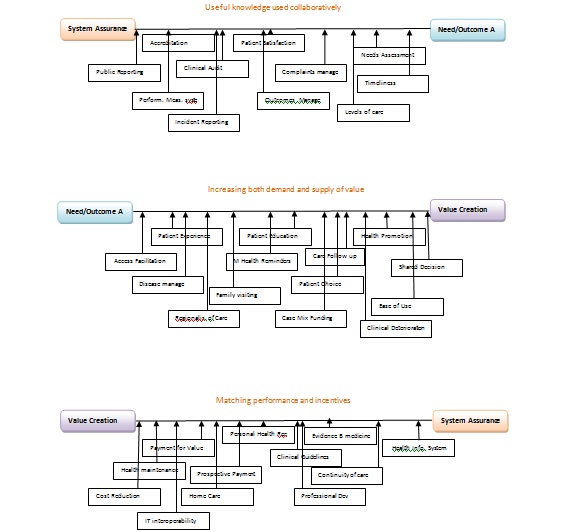
iHQ’s Capability System.
The relations between micro, meso and macro systems is not transitive. The players are different and the incentives are different. The microeffectiveness and macro effectiveness may even be contradictory. However , the capabilities can be shared without cost .
 Campaign’s Improvement Capability Model The model is ultimately about improvement. How to ensure that Mumbai healthcare provides access to safe and quality healthcare at an affordable cost. Such an agenda is not new. What is new is the focus on the system, a forum for synergy and in providing people in the system with the required capabilities. The capabilities will outlive the campaign.
Campaign’s Improvement Capability Model The model is ultimately about improvement. How to ensure that Mumbai healthcare provides access to safe and quality healthcare at an affordable cost. Such an agenda is not new. What is new is the focus on the system, a forum for synergy and in providing people in the system with the required capabilities. The capabilities will outlive the campaign. 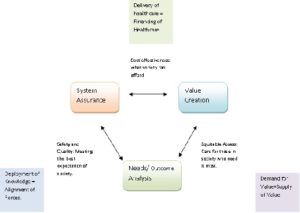
Campaign Infrastructure
Micro-effectiveness and macro- effectiveness infrastructure. However given the current status of healthcare quality in India, organizations would require both internal infrastructure such as trained personnel as well as external infrastructure such as shared data and benchmarks. The campaign is committed to providing both in a focused and affordable manner.

The Capability Manifesto: Quality as capability.
We often tend to view capability as quality. Yet quality is a current state, not something in the future. Capabilities are the conditions that make improvement possible. Capability is ability of a system. More specifically it is the ability/ attributes of the outcomes. Here, Quality is not used in terms of outcomes [ it should already be obvious that quality is not a process but an outcome . The control chart for example always plots outcomes] but as the pursuit of the basics. Thus capability is the answer to the question: What are the goals of healthcare? This can be reinterpreted as : What is it that the public values about healthcare ?
Improvement Science is not merely about the implementation of evidence , the ratification of ideas or the survival of organisations. It is about the ‘validation of healthcare.’ It is the answer to the fundamental question : Does healthcare work? Improvement science is about creating the ‘critical space’. It is the ‘critical theory’ of healthcare. Critical not in terms of negative or even constructive criticism but in ‘elucidating the conditions for the possibility of healthcare’. If healthcare works , then what are the conditions that make it work. The word ‘critic’ has this transcendental notion since the time of Kant. Charles Sanders Pierce who introduced the notion of ‘ abduction’ was so enamoured of Kant’s ‘The Critic of Pure Reason’ that he is said to have spent several hours daily reading it and is believed to have known it by-heart.
If one is uncomfortable with the idea that healthcare actually requires any justification , it is important to scrutinise the relationship between health and healthcare. The sociology of health literature has questioned this relationship which most healthcare professionals have taken. Improvement science is in ‘essence’ the study of the ‘problematic’ of healthcare.
Capabilities treat processes / systems/ communities as resources. It is a ‘patterned activity’ not an ‘ one –time, idiosyncratic change in resource base’.
Capabilities view processes and systems along a maturity model. It is not a grading process but a graduation process.
Capabilities define processes in the future state : unlike flow charts that represent current perception. As potentials they are presystemic .
They are supra-sytemic and meta –systemic. Being presystemic and metasystemic they are understood as design. Thus can be decomposed into logical and conceptual and physical components .
Organization currently do not manage capability: they think in terms of strategies and tactics. Capability is a systemic view point .besides strategic management and operations management they need capability management.
Greater sensitivity to culture , context ,belief systems , values unlike the engineering model of process management [ efficiency / effectiveness]and technological model of creativity[ modernity] and the testimony model of evidence based medicine.[ technical rationality]. Capabilities provide a thicker description of processes .
Capability determines how and whether ‘healthcare systems’ are utilized. This uitilization perspective is in contrast to the resource – based perspective of infrastructure development and system development. The key issue in developing countries is underconsumption of healthcare [ different from developed countries ] and when they consume they are overconsumers of therapy [ whether good or harmful ]and under consumers of prevention.[not different from developed countries].
Capability approach makes improvement local , specific and contingent . At the same time is not merely additional effort . It is a process of democratizing excellence.
Not limited to the inputs and outcomes but what happens in the ‘encounter ‘= how and how the needs are met. Thus sustainability , spread , participation of user , disparity redressal are not add-ons but built within the a wide- angle view of the process design.
Capability approach lends itself to a. to provide situation analysis b. identify the frame work for evaluation and methods and tools for improvement.
Views the consumer of healthcare as “ ‘learning’agent rather than patient “.
Capabilities deconstruct currently prevalent ‘Resources bias’: resource rich therefore capability rich. Similarly, because of poor resources they view their capabilities as poor. The fallacy arises because we tend to see all resources as purely ‘given’ and fail to recognise that there can be resources that are merely ‘derived’ resources . Capabilities thus creates a context of resourcefulness. A new definition of accountability.A defiance of victim mentality. The default state is resource poor / capability rich. The developed countries are resource rich / capability rich. There is no condition of capability poor that is natural . Thus there is merit in using resources to increase functioning or capabilities. To do that ,what needs to be altered is opportunity. Opportunity is not capability. Effective opportunity with effective change is systemness.
Resources are not a given – they are always finite. Capability is used to create resources. Abundant Resourcefulness.[limited resources+ adequate imagination]
Idea of opportunities that are not given but constantly ‘divined’. They can be designed or discovered.
Capability consists of effectiveness[achievement or accountability] and agency[freedom or opportunity]. Effectiveness achievement and effectiveness freedom/agency achievement and agency freedom.
What kind of opportunity and what kind of change? It is change- oriented opportunity.
The path from opportunity to systemness is not linear. You can’t see systemness from opportunity but is ‘u’ process. The process is a fractal. The U-process between opportunity and change and further between change and systemness. Current methodologies of improvement science are focused on the C-S Process.
Systemness warrants spread and sustainability.
The entire process is a emergence . The systemness is embryonic in the opportunity and gets modelled by change. It moves from being – knowing – doing and having. Requires a philosophy of the present[ opportnunity ] and a philosophy of the future[ systemness] , not merely a philosophy of change .
Capability operates beyond supply and demand, unlike cost-cutting.
Capability is context sensitive.Not context determined. There are no problems but only problem situations. To transform you have two options: problem oriented or solution oriented. Opportunity is solution oriented. Problem orientation is structural in evaluation and implementation. Solution orientation is functional in evaluation and implementation. Capability is the ability to find valuable solutions to problems of your choice. A a- historical view of improvement as a right. It is a ‘patterned activity’ not an ‘ one –time, idiosyncratic change in resource base’.
Improvement is a validated capability. Quality is validated opportunity and validated change. You can have improvement without quality but not quality without improvement. All change is not improvement and all improvement is not quality. Improvement science is improvement by quality. There are other ways of improvement: technology,policy, resources, regulation, rules, placebo, hawthorne.
Improvement by quality can be strategy based or capability based. Strategy[ not alone , it must degenerate into work] can be capability and capability can be strategy[ ie strategic capability ].
The chain of effect moves from small to big , local to global , present to future.
Complexity of the past and the complexity of the future.
The time span of opportunities[ window of opportunity] is different across the chain of effects . It is constrained/ fleeting in microsystem but allows for long-term thinking in the macro-system.
The question is not whether there are methods for increasing opportunity , but whether all methods of improvement increase opportunity. All change is not isolated action, but change has a pretext. Opportunity infuses meaning to change.
Strategy matrix
Opportunity Change Systemness
Knowledge of Discipline + ++
Knowledge of Improvement + +++ ++++
Evaluation ++ +
EBM +++ ++
Implementation Science ++ +++ ++
CME +
Research ++
Method model matrix
Scenario planning ++++ + +
Strategy Planning ++ + +
Healthcare Improvement Index: that widens the narrative of improvement to include opportunity. The Improvement Life cycle : Opportunity – Change – Systemness.
Systemness is the wellbeing or flourishing of systems. Currently they are evaluated narrowly in terms of outcomes such as effectiveness and stability of processes.There is a need to go beyond the input – out models. In developing countries all the more relevant as the mere availablity of a resource does not guarantee its use. Thus there is a need to understand utilization as a system problem.
The improvement milieu
Improvement is complex . Not just healthcare or medical knowledge.
Also used as a descriptive tool to understand why some improvement initiatives succeed and others fail .More importantly why improvement science is not yet in vogue in developing , why certain professional groups or even certain individuals in particular are enthusiastic. The effectiveness of participatory resources.
Comparison for capability can be used to adjust effectiveness and enhance adoption of best practices. For example , the efficacy of rrt’s should be consider under framework of the severity of patients on the floors, the nurse patient ratio, the proximity of critical units and the availability of ICU beds , the expertise of general staff in CPR.
For quality to be professional rather than the mechanism of management control of the professions. Allowing the mastery the professional’s value or/and the outcomes the patients desire.
Dimensions of Healthcare Quality Comment
Access Cost Safety Timeliness Effectiveness Equity /gender etc. Capability sets chosen in the system.
Design-achievement Effectiveness
Design freedom Opportunity
Agency achievement Effectiveness
Agency freedom Opportunity
Systemness is a composite but not necessarily unscrutable. It can be defined and measured depending on the chosen capability- sets within that system. Not only capture the design achievement [or design quality] as well as agency achievement or performance quality , but also include two other elements of agency freedom or choice/autonomy and final what is often ignored access/ right to design that is crucial factor in engagement . The famous expression “ every system is designed to get the results it gets “ makes sense only because we have assumed a framework that does not include design freedom. eg. in manufacturing industries, the production department cannot change the design. It could equally be expressed as ‘no system can be designed to produce anything other than what it is designed for “. In this case, the tautology falls apart. Therefore all systems must be designed.
Problem situation vs problems.Most problems in daily work-life have obvious solutions. What problem situation requires to stand back and study the ‘solution’. How far should we go back . This problem ,or the same problem earlier .
Capability and Learning
Learning is part of improvement. However, there is a subtlty involved in capability . It is the difference between ‘learn about’ and ‘learning to be’. Capability is ‘learning to be’. Capability is not the mere ability to do something but to make something, to become something. Learning to learn is a learnable capability.
Capability and Improvement.
Capability is about creating the conditions for improvement. However, improvement itself can create capability. Thus capability can also be seen as effects. While outcomes are ‘downstream effects’ , capability are ‘upstream effects’. The relation between capability and outcomes is nonlinear and linked by methods. Capability is quality before method.
Capability and Competence
Competence is about the past. Capability is about the future i.e an ability in new situations. Capability is heutological. It is not built on certainty but on openness. The nature of collaborative knowledge is rhizomatic. Why is not a mere ability ? Just because you know you cannot do. There are interdependent , external necessary and sufficient conditions. It does not start small and grow. All its necessary and sufficient conditions must be present. Capability Maturity is merely additional. Capability is not the degree of match between theory and practice , but the conditions that allow theory and practice to come together. Capability is about sufficient conditions, though in ordinary parlance it is tempting to view them as merely necessary conditions.
Capability and Process.
A process is resource dependent .Capability is about resourcefulness. Capability is a creative progress. Processes are driven by causes. Capability by possibility. Capabilities are free.
Capability and System
Capability is the ability of the system to meet the needs . As needs will change , capability remains a ‘ongoing process’ rather than a fixed, ‘once and for all’ system. It is systemic , not a science.It is an micro- macro assemblage.
Equating hospitals with healthcare is a category mistake. Capability is a property of the community not the system.
Capability and Quality.
Capability is a common or public good: Unlike Quality which is a competitive good, Capability is a collaborative good. Quality is driven be demand and supply. Capability is free from economics: ‘opportunity and capability’ replace ‘demand and supply’. Capability is the ‘socialisation of quality’.
Capability stays: Capability prioritizes sustainability and spread.
The maturity model thinking is attributable to Crosby : quality management maturity grid.
From Systems to Lifeworlds.
The true venue of healthcare quality is the community . Systems thinking, if taken seriously, requires that we acknowledge the community and not merely ‘the system’. Healthcare is always a subsystem of society. Without community there are several dimensions eg equity that cannot be optimised. This cannot be approached by incrementalism or rolling up but only by flipping healthcare.
The patient- centered movement as located within systems is likely to be shortlived. For one , it operate against the gravity of human psychology. It is impossible for the person who knows and who has worked to get there to be at the beck and call of the patient. It merely offers a ‘romantic view’ of the market. In the largely mechanised world of manufacturing , Deming’s call to include the customer in the system was indeed revolutionary. The problem in medicine was not that the patient was outside the system. So let us step back and understand the problem we are trying to solve with ‘patient centeredness’.
Non of the quality guru’s with a possible exception of Genuchi Taguchi were concerned with societal costs. Deming, so to speak, explicitly equated the market to the world. In the adoption of improvement methodologies the ‘target problem’ was variation or specifically ‘unwanted variation’. With Patient Centeredness , even if we treat it as a extension of ‘customer focus’ the target problem is the lack of ‘ wanted variation’ or customisation. However, Medicine’s ontological challenge is that it is hyper-personal. We now even have genomic personalisation. So the problem that patient centeredness is setting out to solve is not a epistemic one of variation but a metaphysical one of gross reductionism. The objectification by the clinical gaze. Of reducing the ‘subject’ to an ‘object’. The patient as a ‘case’ , ‘case number’ or simply a thing. Merely , co-opting the patient in co-design, in decision-sharing of process are insufficient as antidotes to ‘depersonalisation’. Empowering patients to go beyond ‘needs’ to ‘wants’ is expecting improvement without change. It addresses itself to the challenge of choice and not the challenge of chance.
The quality improvement movement in healthcare had four legacy domains to address but did not do equally well. The first was the polemic with ‘quality assurance ‘ which it found easy to do. It however did not do as well in engaging with the legacy of evidence based healthcare. It was at best apologetic. There were limited attempts to ‘integrate the methodologies’. The third domain is the domain of care. Here again , it has made minimal impact . The agenda ahead is the need to ‘integralise care’. The fourth domain is the community . The agenda ahead is the ‘socialisation of quality’. These charactersiations are merely from the point of view of the discipline of Improvement Science.
This post is limited to issues relating to the third and fourth domains. At the risk of crude summarisation I wish to re-allocate these two domains to the concept of microworlds thus : Micro-life worlds and Macro-lifeworlds. Drawing inspiration from Herbert Marcuse’s complaint of the world becoming ‘one dimensional’, I am suggesting that micro lifeworlds are best constituted by the ‘aesthetisation of the personal ‘ while the macro lifeworlds by the ‘aesthetisation of the social’. In an interview quite late in his career Donabedian identified the ‘aesthetics of care’ as the final frontier of healthcare quality. Improvement Science in its leap to legitimisation has unfortunately neglected the indispensable role of the art. In the second edition of a classic book on improvement, the authors retitled a chapter ‘ The Science and Art of Improvement’ and foregrounded it as merely ‘The Science of Improvement’. I prefer the first.
Prof. Dave Gustafson was among the earliest champions in flipping healthcare. He systematically shifted the focus from patient satisfaction to patient needs or even simply preferences. The idea of undertaking ‘patient journeys’ by literally having himself moved around in a gourney holding a video cam is part of the healthcare improvement folklore. Soon enough there were hospitals that figured out that patient spend most of the time in the supine habitus and had their ceiling covered with paintings rather than have them on the walls. The term aesthetics acquired its connotation of being related to art only in the 18th century, with the work Baumgarten. Interestingly , he was attempting to create a ‘ science of art’. The original connotation derived from the ancient Greeks was aesthesis or sensation or experience. The word anaesthesia is merely its apposite, the absence of sensation. In attributing aesthetisation to the life-world I have still to explain for intersubjectivity. This is the original move from the early to mature Husserl: Phenomenology as a non-empirical science founded on absolute subjectivity to the lifeworld of intersubjectivity. Without wading too deep into philosophical waters one does find scope for universal intent in subjectivity in the Kantian notion of ‘sensus communis’.
The demand for more time , more civility, more role in decision making etc are not issues to be negotiated at the level of the doctor-patient relationship but at the level of value expectations of the community. The system will be strained as unlike the ‘efficiency initiatives’, the ’empathy initiatives’ do not have any potential to reduce workloads. Secondly, medicine and caring professions have always been patient centered and have arisen only because there were people with compassion for the needy. Besides, the patient is also member of the community and ‘sick role’ is only a temporary and temporal identity. It is important to look at the ‘patient’ always as part of the community. For this we need alternative ontologies of caring , we need ‘open hospitals’ ie hospitals without walls. Merely , instrumentalising compassion is not enough.
We need to empower communities not patients. It takes a community to keep a person healthy. The capabilities for quality are not built within systems but within communities. Systems constitute only the supply- side of the equation. The demand for quality, value, safety , sustainability or cost effectiveness has to come from society.
The current formulations of population health actually is about the system acting upon the population. What is required is not community based healthcare but community led healthcare.
